Subscribe, Connect, Learn, Grow:Our Monthly Newsletter Delivers Care Industry Innovation, Critical News, and Insights
NDIS Software Tour
Choose your own journey!
A personalised walkthrough that highlights the CareMaster features most important to you
 Start the Tour!
Start the Tour!


7000+ App Downloads
4.6 Based on 2.6k Reviews
Accurate documentation and record keeping play a key role across a number of facets in aged care settings. As an aged care provider, compiling thorough documentation is not only a legal requirement but an essential step in maintaining compliance with the Aged Care Quality Standards. Not to mention, documentation also provides the foundation for effective communication, allowing you to convey relevant information to and from multidisciplinary team members, health professionals, and family members.
While there are a number of different types of documentation and health records that should be recorded in aged care settings, we’ll be focusing on the main 5 types of documentation in aged care.
A care plan is a detailed document that outlines the specific care needs of an individual, including medical, emotional, social, and daily living support. It’s created in consultation with the elderly person, their family, and healthcare professionals to ensure a person-centred care approach.
These care plans act as a guide for medical and care professionals, detailing how to care for each individual patient. Effective care plans are comprehensive documents that provide information and shared knowledge on medication and exercise and specifics about how they prefer their tea or even how their food should be prepared. That way, doctors, healthcare workers, staff members, and aged care providers have the information they need to ensure the patient receives tailored care without having to ask for information.
When it comes to documenting care plans, it’s important to ensure changes and updates can be easily documented. From adjustments in medication and other details, care documents are constantly evolving to ensure the patient’s care needs are met. Workers should be able to access and enter progress notes for each patient to ensure their care needs are met.
Health records document the patient’s conditions and medical history, medications, treatments, and any medical procedures they’ve undergone. They include a range of different documents and information, including medical assessments, clinical summaries, x-rays, and clinical photos.
Detailed health and medical records ensure healthcare professionals and care workers have access to accurate, up-to-date information about a resident’s health status, medical history, and ongoing treatment. This helps in providing consistent, personalised, and safe care that meets the individual needs of each resident.
Despite everyone’s best efforts, accidents and injuries happen from time to time in aged care settings. Whether a resident has taken a tumble or there are more serious allegations at play, aged care providers must meet their legal requirements in terms of notifying the Aged Care Quality and Safety Commission of any reportable incidents.
As part of their record keeping obligations, organisations offering aged care services must implement an incident management system to record any accidents, injuries, or unusual occurrences involving residents. Incident reports are crucial for identifying risks and implementing measures to prevent future incidents, ensuring the safety of aged care residents.
To provide safe patient care, aged care providers must keep detailed records of their care recipients’ medical documentation. MARs document the administration of medications to residents, including dosage, frequency, and any adverse reactions. Accurate and timely medication documentation is critical for managing residents’ health and avoiding errors in drug administration.
Medication charts and records ensure that medications are administered safely, reduce the risk of errors, and allow for proper monitoring of the resident’s response to treatment in aged care settings.
Progress notes are essential legal documents for aged care providers, as they are required to secure funding subsidies. These notes provide detailed records of a resident’s care and highlight any significant changes in their health. Updated daily, progress notes facilitate communication among caregivers, ensuring everyone is informed about the resident’s condition. Without this documentation, providers can’t obtain the necessary funding support.
Aged care providers in Australia must meet rigorous accreditation standards set by the Aged Care Quality and Safety Commission, which includes maintaining essential documentation related to audits, staff training, safety checks, and regulatory compliance. Under the Aged Care Act 1997 (Cth), providers must keep paper-based or electronic records to demonstrate adherence to these standards.
Due to the nature of the services and supports offered by aged care providers, they’re often classified as healthcare organisations. As such, aged care services must comply with strict record keeping regulations that apply to healthcare organisations. For patient care recipients who have received a health service, records must be kept for a minimum of seven years and, in some cases, up to 25 years. This aligns with privacy laws such as the Privacy Act 1988 and various state and territory privacy regulations, which set specific rules for securely storing patient information.
Thorough documentation is essential for effective communication across services and proof that a provider operates in line with the Eight Aged Care Quality Standards and meets the requirements of a triennial quality review. In addition, to qualify for government funding subsidies under the Aged Care Act, providers must meet several criteria, including the documentation requirements outlined in Part 7A of the Aged Care Quality and Safety Commission Act and the Eight Aged Care Quality Standards.
Ultimately, documentation allows aged care services to provide quality care and support services to your patients. Aged care providers in Australia are legally required to keep detailed and accurate records under the Aged Care Quality Standards. These records are vital during audits and inspections by regulatory bodies, ensuring that facilities meet safety, care, and ethical standards.
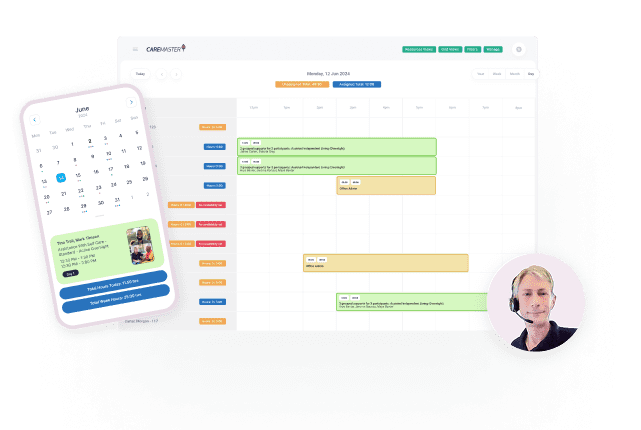
The key to developing good documentation and record keeping is to store everything in a centralised, electronic document management system that can be easily accessed and updated by the patient’s healthcare team. At CareMaster, our aged care software provides an all-in-one solution for all parties, including aged care services, health service workers, and care workers. Our platform allows you to securely store detailed aged care documentation, records, and observation notes while providing easy access to relevant workers.