Subscribe, Connect, Learn, Grow:Our Monthly Newsletter Delivers Care Industry Innovation, Critical News, and Insights
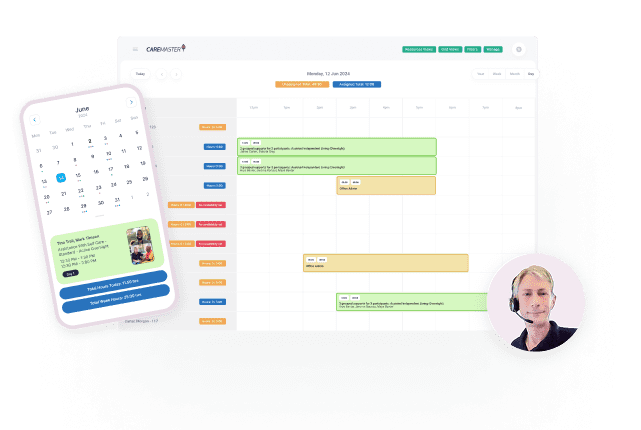
NDIS Software Tour
Choose your own journey!
A personalised walkthrough that highlights the CareMaster features most important to you
 Start the Tour!
Start the Tour!


7000+ App Downloads
4.6 Based on 2.6k Reviews
The latest State of the Disability Sector Report 2025 results concerning and highlight some of the real problems within the sector. Whilst I absolutely agree the NDIS needs to be fiscally sustainable and ensure fraud is not rife, this report highlights some of the real challenges of providers, especially those doing the right thing, getting registered and essentially providing unfunded services for free.
Providers, particularly those doing the right thing, are being pushed to breaking point.
We need to remember, instead of getting caught up in endless media reports and political narratives, that the real risk given this report, is that participants, many of whom are vulnerable, along with their families and support networks, are the ones who in the end will be impacted if more and more providers go out of business.
A system being propped up by unfunded work
The data is grim. Nearly half of disability service providers reported a financial loss in 2024–25, and 81 per cent say they cannot continue delivering services at current NDIS prices. This is not about inefficiency; it demonstrates structural strain.
More concerning is the scale of unfunded services now embedded in “business as usual”:
77 per cent of providers delivered unfunded supports last year
At an average cost of more than $460,000 per organisation
Totalling over $69 million across the sector
These unfunded supports include crisis response, support coordination, bridging gaps when plans are exhausted, travel, system navigation, and keeping people safe when the funding simply doesn’t line up.
Put plainly, providers are subsidising the system to protect participants, at their own expense.
Many are quietly absorbing costs until they can’t anymore, unsurprising then that hundreds of smaller provider closures reported sector-wide, along with even larger providers like Centacare Queensland (withdrew NDIS-funded disability services, affecting ~700 clients and ~600 staff), Bedford Group (entered voluntary administration as a major disability employment services provider), and NDISP (specialist disability accommodation company shut down operations).
Doing the right thing costs more
Registration, quality and safeguarding matter. They protect people. But the current settings mean registered providers carry significantly higher compliance costs while receiving the same pricing as unregistered providers.
Providers report that compliance and audit requirements are resource-intensive, unclear at times, and not proportionate to risk, yet they remain committed to meeting them because quality and safety matter.
This creates an interesting dichotomy. Providers who invest in quality, training, audits and governance are financially penalised. Whereas unregistered Providers are often more commercially viable, despite Participants are exposed to greater risk over time.
When providers disappear, participants pay the price
In 2025 the sector has seen well-known, large providers exit the market, following several years of deteriorating financial performance. These were not small operators; they were organisations delivering services at scale, employing hundreds of workers, and supporting thousands of participants.
Each closure means Participants lose trusted supports; families scramble for alternatives and workers lose jobs.
Remaining providers absorb demand they are already struggling to meet.
The report shows 77 per cent of providers are already turning away people who need support, due to workforce shortages, capacity constraints and funding gaps.
If more providers go under, this problem compounds. Continuity of care suffers, especially for people with complex needs, in regional areas, or requiring consistent relationships.
This is the real risk hidden behind the headlines.
Providers are trying to adapt — but it’s not enough
Despite the pressure, providers are not standing still.
More than 90 per cent are actively trying to improve productivity, many through digital transformation, better use of data and streamlining operations.
But the same report and our own customer research, show that many providers are hitting a ceiling. Manual processes, duplicated systems and administrative overhead are eating into already thin margins.
Our customer research with NDIS providers ranging from 20 to over 500 staff found consistent themes:
Heavy reliance on spreadsheets and workarounds
Manual payroll, billing and reconciliation consuming hours every week
Rostering knowledge concentrated in one or two people
Compliance risks created by poor permissions and data validation
Staff spending time fixing errors instead of supporting participants
In one case, a mid-sized provider reported eight hours a week spent manually processing payroll. Another was three months behind in billing, creating real cash-flow risk. Several described full days each week spent cleaning up data entered incorrectly. This is not a failure of effort. It is a failure of systems.
Technology isn’t the answer — but it is part of it
This is not about spruiking software, or pretending technology alone can fix structural funding issues. It can’t.
But there is a clear opportunity to reduce the cost of compliance, cut administrative waste, and give providers back time, if technology is applied innovatively and intelligently.
During customer research sessions, providers were very clear about what they needed.
Better data validation to prevent errors before they happen
Automated workflows that enforce compliance without manual policing
Smarter rostering that balances participant needs, worker skills, fatigue and availability
Tools that support quality documentation rather than chasing it after the fact
AI that assists decision-making, not replaces human judgement
When done well, this directly supports sustainability — not by cutting corners, but by removing friction.
What we’ve seen work in practice
Through direct customer research and industry consultation, we’ve seen how the right tools can make a tangible difference.
At Community Accessibility, a large provider onboarding more than 200 participants a month, teams described spending “hours on the phone” manually trying to backfill shifts when multiple staff called in sick. Improving rostering visibility and automation reduced pressure on both staff and participants.
At Community Accessibility they noted “at this scale, spreadsheets are a liability, not a workaround”
Across multiple organisations, providers reported:
Payroll and billing processing reduced from hours to minutes
Rostering no longer reliant on a single “indispensable” staff member
Built-in checks preventing funding exhaustion before services are delivered
Clear audit trails reducing compliance risk and stress
Staff spending less time fixing mistakes and more time with participants
Importantly, these improvements don’t change what providers do best. They free them up to focus on care, relationships and outcomes.
Conclusion
The NDIS does need to be sustainable. Fraud does need to be addressed. But sustainability cannot be achieved by squeezing compliant providers until they fail. If the current trajectory continues, the data is clear, and participants will be the ones who pay the price through fewer services, less choice, disrupted care and increased risk.
Supporting providers to navigate compliance, reduce administrative burden and use technology wisely is a necessary part of protecting the integrity of the scheme and the people it exists to support.
At CareMaster, our purpose is simple: to empower our community to live the life they want, and to support providers to deliver excellent care without burning out or going broke trying to do the right thing.
Authored by Elisha Anderton
Chief Operating Officer, CareMaster
Source: National Disability Services (NDS), State of the Disability Sector Report.
https://nds.org.au/about/state-of-the-disability-sector-report